Masquelet technique to treat a septic nonunion after plating of a femoral open fracture
Masquelet Technique
Abstract
Septic nonunion is one of the most common complications after an open fracture . Risk of infection and bony defect are common after open fracture . So we need to dealt with both to improve patient outcome .
Treatment is always complicated and expensive and there is an uncertainty in the final outcome .
In 1980’s, Masquelet first described the technique of the induced membrane and autologous bone grafting to manage critical size bone defects.
In Septic non-union 2 diffenrent surgical steps are require for management .In former step , allow radical management to control infection and in later step , allow biological stimulus for bone healing .
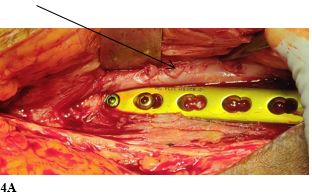
In this case , we present a 28 years old female patient with open grade 3A Femur shaft Fracture on right side . Patient was initially treated with wound debridement and Femur plating which unfortunately resulted in septic non-union .It was then subsequently managed with the induced membrane technique and a double-plate osteosynthesis to protect the biological chamber.
Downloads
References
Mills L.A., Aitken SA, Simpson A. The risk of non-union per fracture: current myths and revised figures from a population of over 4 million adults. Acta Orthop 2017;88:434–9.
[2] Simpson AH, Tsang JST. Current treatment of infected non-union after intramedullary nailing. Injury 2017;48(Suppl 1):S82–s90.
[3] Hak DJ, Fitzpatrick D, Bishop JA, Marsh JL, Tilp S, Schnettler R, et al. Delayed union and nonunions: epidemiology, clinical issues, and financial aspects. Injury 2014;45(Suppl 2):S3–7.
[4] El-Gammal TA, Shiha AE, El-Deen MA, El-Sayed A, Kotb MM, Addosooki AI, et al. Management of traumatic tibial defects using free vascularized fibula or Ilizarov bone transport: a comparative study. Microsurgery 2008;28:339–46.
[5] Masquelet AC, Fitoussi F, Begue T, Muller GP. [Reconstruction of the long bones by the induced membrane and spongy autograft]. Annales de chirurgie plastique et esthetique 2000;45:346–53.
[6] Zura R, Xiong Z, Einhorn T, Watson JT, Ostrum RF, Prayson MJ, et al. Epidemiology of fracture nonunion in 18 human bones. JAMA Surg 2016;151: e162775.
[7]Santolini E, Goumenos SD, Giannoudi M, Sanguineti F, Stella M, Giannoudis PV. Femoral and tibial blood supply: A trigger for non-union? Injury 2014;45:1665–73.
[8]Gelalis ID, Politis AN, Arnaoutoglou CM, Korompilias AV, Pakos EE, Vekris MD, et al. Diagnostic and treatment modalities in nonunions of the femoral shaft: a review. Injury 2012;43:980–8.
[9] Winquist RA, Hansen Jr. ST, Clawson DK. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Joint Surg Am 1984;2001(83-a):1912.
[10] Wolinsky PR, McCarty E, Shyr Y, Johnson K. Reamed intramedullary nailing of the femur: 551 cases. J Trauma 1999;46:392–9.
[11] Nandra R, Grover L, Porter K. Fracture non-union epidemiology and treatment. Trauma 2015;18:3–11.
[12] Papakostidis C, Kanakaris NK, Pretel J, Faour O, Morell DJ, Giannoudis PV. Prevalence of complications of open tibial shaft fractures stratified as per the Gustilo-Anderson classification. Injury 2011;42:1408–15.
[13] Thakore RV, Francois EL, Nwosu SK, Attum B, Whiting PS, Siuta MA, et al. The Gustilo-Anderson classification system as predictor of nonunion and infection in open tibia fractures. Eur J Trauma Emerg Surg 2017;43:651–6.
[14] Elniel AR, Giannoudis PV. Open fractures of the lower extremity: current management and clinical outcomes. EFORT Open Rev 2018;3:316–25.
[15] Kanakaris NK, Tosounidis TH, Giannoudis PV. Surgical management of infected non-unions: an update. Injury 2015;46(Suppl 5):S25–32.
[16] Zhang Q, Zhang W, Zhang Z, Zhang L, Chen H, Hao M, et al. Femoral nonunion with segmental bone defect treated by distraction osteogenesis with monolateral external fixation. J Orthop Surg Res 2017;12:183.
[17] Calori GM, Colombo M, Malagoli E, Mazzola S, Bucci M, Mazza E. Megaprosthesis in post-traumatic and periprosthetic large bone defects: issues to consider. Injury 2014;45(Suppl 6):S105–10.
[18] Lindsey RW, Gugala Z, Milne E, Sun M, Gannon FH, Latta LL. The efficacy of cylindrical titanium mesh cage for the reconstruction of a critical-size canine segmental femoral diaphyseal defect. J Orthop Res 2006;24:1438–53.
[19] Ronga M, Ferraro S, Fagetti A, Cherubino M, Valdatta L, Cherubino P. Masquelet technique for the treatment of a severe acute tibial bone loss. Injury 2014;45 (Suppl 6):S111–5.
[20] Woon CY, Chong KW, Wong MK. Induced membranes–a staged technique of bone-grafting for segmental bone loss: a report of two cases and a literature review. J Bone Joint Surg Am 2010;92:196–201.
[21] Masquelet AC. Induced membrane technique: pearls and pitfalls. J Orthop Trauma 2017;31(Suppl 5):S36–s8.
[22] Azi ML, Teixeira AA, Cotias RB, Joeris A, Kfuri Jr. M. Membrane induced osteogenesis in the management of posttraumatic bone defects. J Orthop Trauma 2016;30:545–50.
[23] Giannoudis PV, Faour O, Goff T, Kanakaris N, Dimitriou R. Masquelet technique for the treatment of bone defects: tips-tricks and future directions. Injury 2011;42:591–8.
[24] Giannoudis PV, Harwood PJ, Tosounidis T, Kanakaris NK. Restoration of long bone defects treated with the induced membrane technique: protocol and outcomes. Injury 2016;47(Suppl 6):S53–s61.
[25] Liu H, Hu G, Shang P, Shen Y, Nie P, Peng L, et al. Histological characteristics of induced membranes in subcutaneous, intramuscular sites and bone defect. Orthop Traumatol Surg Res 2013;99:959–64.
[26] Pelissier P, Masquelet AC, Bareille R, Pelissier SM, Amedee J. Induced membranes secrete growth factors including vascular and osteoinductive factors and could stimulate bone regeneration. J Orthop Res 2004;22:73–9.
[27] Gruber HE, Ode G, Hoelscher G, Ingram J, Bethea S, Bosse MJ. Osteogenic, stem cell and molecular characterisation of the human induced membrane from extremity bone defects. Bone Joint Res 2016;5:106–15.
[28] Olesen UK, Eckardt H, Bosemark P, Paulsen AW, Dahl B, Hede A. The Masquelet technique of induced membrane for healing of bone defects. A review of 8 cases. Injury 2015;46(Suppl 8):S44–7.
[29] Jiang Y, Guo YF, Meng YK, Zhu L, Chen AM. A report of a novel technique: the comprehensive fibular autograft with double metal locking plate fixation (cFALP) for refractory post-operative diaphyseal femur fracture non-union treatment.
Copyright (c) 2023 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


















 Therapoid
Therapoid

