A clinical study to predict the outcome of patients with hollow viscus perforation in a tertiary care hospital using manheim peritonitis index
Abstract
Introduction: Since a longtime multiple effort are been put forwarded to design an effective scoring system as to predict the outcome as to mortality and morbidity of patients admitting to hospitals with hollow viscus perforations. Of number of proposed systems Mannheim Peritonitis index is quite simple and effective scoring system proposed to predict the outcome of the patients admitted to hospital with hollow viscus perforations.
Objective: To assess the validity of Mannheim Peritonitis Index (MPI) for predicting the surgical outcome, mortality and morbidity of cases presenting with Hollow viscus perforation.
Method: Current prospective study was one over a period of three years form 2014-2017 at Department of Surgery, Government Medical College, Anantapuramu and included 100 cases between 17-46 years of age.
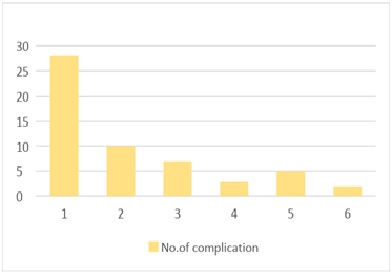
Results: The results of the current study indicated that duodenal perforations are common amongst the hollow viscus perforations, clear exudates were common among peritonitis cases. about 50% of cases presented with postoperative complications. Subjects fitting into MPI scores between 22-29 presented with surgical site infections. higher MPI scores are associated to higher ICU stays. Higher score are observed in cases with feculent and purulent exudates and in turn to relatively more number of complications.
Conclusion: The Mannheim Peritonitis index provide a novel and excellent platform as to predict the surgical outcome, mortality and morbidity in cases of hallow viscera perforations with peritonitis with all associated issues related to the conditions.
Downloads
References
2. Moller MH, Engebjerg MC, Adamson S, Bendix J, Thomsen RW. The Peptic Ulcer Perforation (PULP) score: a predictor of mortality following peptic ulcer perforation. A cohort study. Acta anaesthesiologicaScandinavica. 2012;56(5):655–62.[pubmed]
3. Moller MH, Adamsen S, Thomsen RW, Moller AM. Preoperative prognostic factors for mortality in peptic ulcer perforation – a systematic review. Scand J Gastroenterol. 2010; 45:785–805.[pubmed]
4. Moller MH, Shah K, Bendix J, Jensen AG, Zimmermann-Nielsen E, Adamsen S, Moller AM. Risk factors in patients surgically treated for peptic ulcer perforation. Scand J Gastroenterol. 2009; 44:145–52.[pubmed]
5. Knaus WA, Zimmerman JE, Wagner DP, Draper EA, Lawrence DE. APACHE-acute physiology and chronic health evaluation: a physiologically based classification system. Critical Care Medicine. 1981:9.[pubmed]
6. [6] Boey J, Choi SKY, Alagaratnam TT, Poon A. Risk stratification in perforated duodenal ulcers. Ann Surg. 1987; 205:22–6.[pubmed]
7. Linder MM, Wacha H, Feldmann U, Wesch G, Streifensand RA, Gundlach E. The Mannheim peritonitis index. An instrument for the intraoperative prognosis of peritonitis. Der Chirurg; Zeitschrift fur alleGebiete der operativenMedizen. 1987 Feb;58(2):84-92.
8. Bohen J, Boulanger M, Meakins JL, Mclean AP. Prognosis in generalized peritonitis. Relation to cause and risk factors. Arch Surg. 1983; 118:285-90.[pubmed]
9. Biling A, Frolich D, Schildberg F. Prediction of outcome using the Mannheim peritonitis index in 2003 patients. Br J Surg. 1994;81:209-13.[pubmed]
10. Smith J, Caldwell E, D’Amours S, Jalaludin B, Sugrue M. Abdominal trauma: a disease in evolution. ANZ journal of surgery. 2005 Sep 1;75(9):790-4.[pubmed]
11. Watts DD, Fakhry SM, EAST Multi-Institutional HVI Research Group. Incidence of hollow viscus injury in blunt trauma: an analysis from 275,557 trauma admissions from the East multi-institutional trial. Journal of Trauma and Acute Care Surgery. 2003 Feb 1;54(2):289-94.[pubmed]
12. Ramachandra ML, Jagadesh B, Chandra SB. Clinical study and management of secondary peritonitis due to perforated hollow viscous. Archives of Medical Science. 2007 Jan 1;3(1):61-8.
13. Pacelli F, Doglietto GB, Alfieri S, Piccioni E, Sgadari A, Gui D, Crucitti F. Prognosis in intra-abdominal infections: multivariate analysis on 604 patients. Archives of surgery. 1996 Jun 1;131(6):641-5.[pubmed]
14. Lohsiriwat V, Prapasrivorakul S, Lohsiriwat D. Perforated peptic ulcer: clinical presentation, surgical outcomes, and the accuracy of the Boey scoring system in predicting postoperative morbidity and mortality. World journal of surgery. 2009 Jan 1;33(1):80-5.[pubmed]
15. Függer R, Rogy M, Herbst F, Schemper M, Schulz F. Validation study of the Mannheim peritonitis index. Der Chirurg; Zeitschrift fur alleGebiete der operativenMedizen. 1988 Sep;59(9):598-601.
16. Gooszen AW, Tollenaar RA, Geelkerken RH, Smeets HJ, Bemelman WA, Van Schaardenburgh P, Gooszen HG. Prospective study of primary anastomosis following sigmoid resection for suspected acute complicated diverticular disease. British journal of surgery. 2001 May 1;88(5):693-7.
17. Demmel N, Maag K, Osterholzer G. The value of clinical parameters for determining the prognosis of peritonitis--validation of the Mannheim Peritonitis Index. LangenbecksArchiv fur Chirurgie. 1994;379(3):152-8.
18. Seiler CA, Brügger L, Forssmann U, Baer HU, Büchler MW. Conservative surgical treatment of diffuse peritonitis. Surgery. 2000 Feb 1;127(2):178-84.[pubmed]
19. Chromik AM, Meiser A, Hölling J, Sülberg D, Daigeler A, Meurer K, Vogelsang H, Seelig MH, Uhl W. Identification of patients at risk for development of tertiary peritonitis on a surgical intensive care unit. Journal of Gastrointestinal Surgery. 2009 Jul 1;13(7):1358-67.[pubmed]
20. Bosscha K, Reijnders K, Hulstaert PF, Algra A, Van der Werken C. Prognostic scoring systems to predict outcome in peritonitis and intra‐abdominal sepsis. British journal of surgery. 1997 Nov 1;84(11):1532-4.[pubmed]
21. Biondo S, Ramos E, Fraccalvieri D, Kreisler E, Ragué JM, Jaurrieta E. Comparative study of left colonic peritonitis severity score and Mannheim peritonitis index. British journal of surgery. 2006 May 1;93(5):616-22.[pubmed]
22. Schoeffel U, Jacobs E, Ruf G, Mierswa F, Farthmann EH. Intraperitoneal micro-organisms and the severity of peritonitis. The European journal of surgery= Acta chirurgica. 1995 Jul;161(7):501-8.[pubmed]


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


















 Therapoid
Therapoid

