A retrospective cohort study of diabetic foot disease during the covid pandemic in a tertiary care hospital in Kerala
Abstract
Introduction: Diabetes affects 88 million people in south-east Asia with a regional prevalence of 8.8%, and of them, 77 million live in India. Diabetic Foot Disease is an important complication that accounts for significant morbidity and mortality in a diabetic individual.
Aim: This study was conducted to study the presentation stage of diabetic foot disease during the pandemic period as seen at a tertiary care hospital in North Kerala.
Methods: This was a retrospective cohort study carried out on patients diagnosed with diabetic foot and admitted to the Department of Surgery of a tertiary care hospital in North Kerala during the study period of 6months from July 2020 to December 2020. A sample size of 63 was calculated. Data were collected from the case records of the patients, and the stages of presentation, relevant blood investigations, culture reports, radiological imaging and arterial doppler ultrasound findings were noted. The status of the patient at the time of discharge was noted.
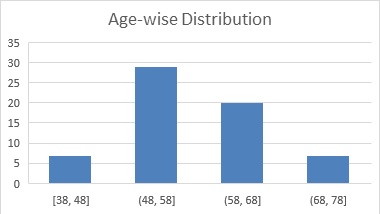
Results: In this study, a total of 63 patients were included. Of the 63 patients, 51(80.9%) were males, and 12 (19.0%) were females with a male to female ratio of 4.25:1. The mean age of the patients was 57.74 years. In this study, as per the Wagner-Meggitt Classification of diabetic foot, the most common stage of presentation of diabetic foot encountered was Grade III (42.9%) followed by Grade IV (28.6%), Grade II (19.0%) and Grade V (9.5%).
Conclusion: This is in part may be due to financial constraints of the patient's families due to lack of job, transportation difficulties, shortage of medicines, shutting down of small scale health care facilities and pharmacies, prolonged neglect of wounds, discontinuing of regular medications and poor home wound care which in turn are due to the frequent regional lockdowns as a result of the covid pandemic.
Downloads
References
International Diabetes Federation. IDF Diabetes Atlas 9th Edition [Internet]; Brussels, Belgium: International Diabetes Federation;2019. Available from: https://www.diabetesatlas.org/upload/resources/material/20191218_144626_sea_factsheet_en.pdf.
International Diabetes Federation. IDF Diabetes Atlas 9th Edition [Internet]; Brussels, Belgium: International Diabetes Federation;2019. Available from: https://www.diabetesatlas.org/data/en/country/93/in.html
Moulik PK, Mtonga R, Gill GV. Amputation and mortality in new-onset diabetic foot ulcers stratified by etiology. Diabetes Care. 2003 Feb;26(2):491-4. doi: 10.2337/diacare.26.2.491.
Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis †. Ann Med. 2017 Mar;49(2):106-116. doi: 10.1080/07853890.2016.1231932.
Amin N, Doupis J. Diabetic foot disease: From the evaluation of the "foot at risk" to the novel diabetic ulcer treatment modalities. World J Diabetes. 2016 Apr 10;7(7):153-64. doi: 10.4239/wjd.v7.i7.153.
Boulton AJ, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J. The global burden of diabetic foot disease. Lancet. 2005 Nov 12;366(9498):1719-24. doi: 10.1016/S0140-6736(05)67698-2.
Unnikrishnan R, Anjana RM, Mohan V. Diabetes mellitus and its complications in India. Nat Rev Endocrinol. 2016 Jun;12(6):357-70. doi: 10.1038/nrendo.2016.53.
International Diabetes Federation. Clinical Practice Recommendation on the Diabetic Foot: A guide for health care professionals [Internet]; Brussels, Belgium: International Diabetes Federation;2017. Available from: https://www.idf.org/e-library/guidelines/119-idf-clinical-practice-recommendations-on-diabetic-foot-2017.html
International Diabetes Federation. IDF Diabetes Atlas 9th Edition [Internet]; Brussels, Belgium: International Diabetes Federation;2019. Available from: https://www.diabetesatlas.org/data/en/world/
Yazdanpanah L, Shahbazian H, Nazari I, Arti HR, Ahmadi F, Mohammadianinejad SE, et al. Incidence and Risk Factors of Diabetic Foot Ulcer: A Population-Based Diabetic Foot Cohort (ADFC Study)-Two-Year Follow-Up Study. Int J Endocrinol. 2018 Mar 15;2018:7631659. doi: 10.1155/2018/7631659.
Joseph EL, Michael LG, Rubinn JP, Christopher GW, Fu-Chan W. Plastic and Reconstructive Surgery. In: Brunicardi FC, Andersen DK, Billiar TB, Dunn DL, Hunter JG, Mathews JB, Pollock RE, editors. Schwartz's Principles of Surgery. 10th ed. New York: McGraw Hill;2015. p. 1877-79.
Musa IR, Ahmed MON, Sabir EI, Alsheneber IF, Ibrahim EME, Mohamed GB, et al. Factors associated with amputation among patients with diabetic foot ulcers in a Saudi population. BMC Res Notes. 2018 Apr 27;11(1):260. doi: 10.1186/s13104-018-3372-z.
Ugwu E, Adeleye O, Gezawa I, Okpe I, Enamino M, Ezeani I. Predictors of lower extremity amputation in patients with diabetic foot ulcer: findings from MEDFUN, a multi-center observational study. J Foot Ankle Res. 2019 Jun 14;12:34. doi: 10.1186/s13047-019-0345-y.
Deerochanawong C, Home PD, Alberti KG. A survey of lower limb amputation in diabetic patients. Diabet Med. 1992 Dec;9(10):942-6. doi: 10.1111/j.1464-5491.1992.tb01736.x.
Wagner FW Jr. The dysvascular foot: a system for diagnosis and treatment. Foot Ankle. 1981 Sep;2(2):64-122. doi: 10.1177/107110078100200202.
Frykberg RG. Diabetic foot ulcers: pathogenesis and management. Am Fam Physician. 2002 Nov 1;66(9):1655-62.
Dinh T, Veves A. The influence of gender as a risk factor in diabetic foot ulceration. Wounds. 2008 May;20(5):127-31.
Abbott CA, Carrington AL, Ashe H, Bath S, Every LC, Griffiths J, et al. North-West Diabetes Foot Care Study. The North-West Diabetes Foot Care Study: incidence of, and risk factors for, new diabetic foot ulceration in a community-based patient cohort. Diabet Med. 2002 May;19(5):377-84. doi: 10.1046/j.1464-5491.2002.00698.x.
Al-Rubeaan K, Al Derwish M, Ouizi S, Youssef AM, Subhani SN, Ibrahim HM, et al. Diabetic foot complications and their risk factors from a large retrospective cohort study. PLoS One. 2015 May 6;10(5):e0124446. doi: 10.1371/journal.pone.0124446.
Hasan, F. A. I. Z. U. L., et al. "Diabetic foot-assessment and management of 100 cases." Pak J Med Health Sci 5 (2011): 677-681.
Farooque U, Lohano AK, Hussain Rind S, Rind MS Sr, Karimi S, Jaan A, et al. Correlation of Hemoglobin A1c With Wagner Classification in Patients With Diabetic Foot. Cureus. 2020 Jul 15;12(7):e9199. doi: 10.7759/cureus.9199.
Farooque U, Lohano AK, Hussain Rind S, Rind MS Sr, Karimi S, Jaan A, et al. Correlation of Hemoglobin A1c With Wagner Classification in Patients With Diabetic Foot. Cureus. 2020 Jul 15;12(7):e9199. doi: 10.7759/cureus.9199.
Forsythe RO, Hinchliffe RJ. Assessment of foot perfusion in patients with a diabetic foot ulcer. Diabetes Metab Res Rev. 2016 Jan;32 Suppl 1:232-8. doi: 10.1002/dmrr.2756.
Bajaj S, Mahajan A, Grover S, Mahajan V, Goyal P, Gupta VK. Peripheral Vascular Disease in Patients with Diabetic Foot Ulcers - An Emerging Trend: A Prospective Study from North India. J Assoc Physicians India. 2017 May;65(5):14-17.
Selvin E, Wattanakit K, Steffes MW, Coresh J, Sharrett AR. HbA1c and peripheral arterial disease in Diabetes: the Atherosclerosis Risk in Communities study. Diabetes Care. 2006 Apr;29(4):877-82. doi: 10.2337/diacare.29.04.06.dc05-2018.
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


















 Therapoid
Therapoid

