A Prospective study on Gastrointestinal Perforation Peritonitis in Andhra Pradesh, India
Abstract
Introduction: Perforation is defined as an abnormal opening in a hollow organ or viscus. All over the world, perforation peritonitis is the most prevalent surgical emergency tackled and treated by a surgical team. The etiology leading to peritonitis in tropical countries shows a different spectrum from its western world. The present study was conducted to highlight the spectrum of hollow viscus perforation peritonitis in terms of etiology, clinical presentations, site of perforation, surgical treatment, postoperative complications, and mortality encountered.
Methods: The study was a prospective observational study conducted from March 2016 to March 2019 in the Department of General Surgery, Great Eastern Medical School and Hospital, Andhra Pradesh. A total of 320 patients with perforation peritonitis were included in the study and underwent exploratory laparotomy.
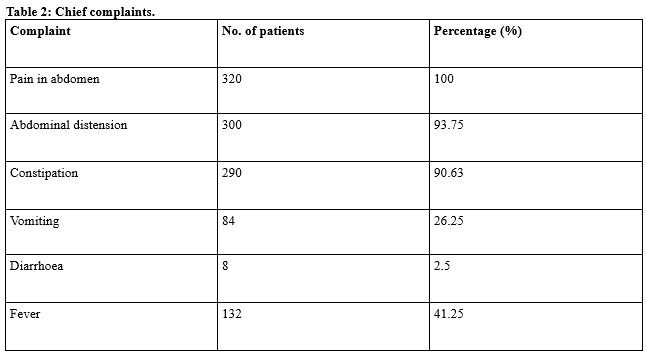
Results: Out of 320 patients, there were 276 males (86.25%) and 44 females (13.75%). Duodenal perforation was the most common type (34.38%), which was mainly due to Acid peptic disease followed by Jejunal and Ileal perforations. Wound infection was the most common complication. The mortality rate was 8.44% (27 patients).
Conclusion: Early diagnosis, resuscitation with fluids, and timely surgical intervention are the most important factors deciding the fate of the patient with perforation peritonitis.
Downloads
References
Ramakrishnan K, Salinas RC. Peptic ulcer disease. Am Fam Physician 2007;76(7):1005-12.
Agarwal N, Saha S, Srivastava A, Chumber S, Dhar A, Garg S. Peritonitis: 10 years’ experience in a single surgical unit. Trop Gastroenterol. 2007;28(3):117-120.
Gupta S, Kaushik R. Peritonitis - The Eastern experience. World J Emerg Surg. 2006;1:13. doi: 10.1186/1749-7922-1-13.
Malangoni MA, Inui T. Peritonitis – the Western experience. World J Emerg Surg. 2006;1:25. doi: 10.1186/1749-7922-1-25.
Afridi SP, Malik F, Ur-Rahman S, Shamim S, Samo KA. Spectrum of perforation peritonitis in Pakistan: ses Eastern experience. World J Emerg Surg. 2008;3:31. doi: 10.1186/1749-7922-3-31.
Dorairajan LN, Gupta S, Deo SV, Chumber S, Sharma LK. Peritonitis in India – A decade’s experience. Trop Gastroenterol. 1995;16(1):33-38.
Jhobta RS, Attri AK, Kaushik R, Sharma R, Jhobta A. Spectrum of perforation peritonitis in India – Review of 504 consecutive cases. World J Emerg Surg. 2006;1:26. doi: 10.1186/1749-7922-1-26.
Sharma L, Gupta S, Soin AS, Sikora S, Kapoor V. Generalized peritonitis in India – The tropical spectrum. Jpn J Surg. 1991;21(3):272-277. doi: 10.1007/BF02470946.
Mahajan G, Kotru M, Sharma R, Sharma S. Usefulness of histopathological examination in nontraumatic perforation of smallintestine. J Gastrointest Surg. 2011;15(10):1837-41. doi: 10.1007/s11605-011-1646-z.
Jain BK, Arora H, Srivastava UK, Mohanty D, Garg PK. Insight into the management of non-traumatic perforation of the small intestine. J Infect Dev Ctries. 2010;4(10):650-654. doi: 10.3855/jidc.829.
Gupta SK, Gupta R, Singh G, Gupta S. Perforation peritonitis: A two year experience. JK Sci. 2010;12(3):141-144.
Ramakrishnaiah VP, Chandrakasan C, Dharanipragadha K, Sistla S, Krishnamachari S. Community acquired secondary bacterial peritonitis in a tertiary hospital of South India: An audit with special reference to peritoneal fluid culture. Trop Gastroenterol. 2012;33(4):275-281. doi: 10.7869/tg.2012.70.
Svanes C, Salvesen H, Espehaug B, Søreide O, Svanes K. A multifactorial analysis of factors related to lethality after treatment of perforated gastroduodenal ulcer 1935-1985. Ann Surg. 1989;209(4):418-423. doi: 10.1097/00000658-198904000-00005.
Wani RA, Parray FQ, Bhat NA, Wani MA, Bhat TH, Farzana F. Nontraumatic terminal ileal perforation. World J Emerg Surg. 2006;1:7. doi: 10.1186/1749-7922-1-7.
Kimchi NA, Broide E, Shapiro M, Scapa E. Non-traumatic perforation of the small intestine. Report of 13 cases and review of the literature. Hepatogastroenterology 2002;49(46):1017-1222.
Sharma MP, Bhatia V. Abdominal tuberculosis. Indian J Med Res. 2004;120(4):305-315.
Afridi SP, Malik F, Ur-Rahman S, Shamim S, Samo KA. Spectrum of perforation peritonitis in Pakistan: 300 cases Eastern experience. World J Emerg Surg. 2008;3:31. doi: 10.1186/1749-7922-3-31.
Chalya P, Mabula JB, Koy M, Mchembe MD, Jaka HM, Kabangila R, et al. Clinical profile and outcome of surgical treatment of perforated peptic ulcers in Northwestern Tanzania: A tertiary hospital experience, World J Emerg Surg. 2011;6:31. doi: 10.1186/1749-7922-6-31
Goud VS, Babu NV, Kumar PB. Comparative Study of Closure of Duodenal Perforations with Omental Plugging Versus Graham’s Patch. Int J Sci Stud. 2016;4(8):138-142. doi: 10.17354/ijss/2016/585.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


















 Therapoid
Therapoid

