An analysis of post-burn problems in patients attending the OPD of a tertiary level care center
Abstract
Background: To analyze post-burn problems of patients and to prepare a protocol and guidelines for the patient and attendants during hospitalization for timely intervention and to prevent the post-burn sequels and therapeutic measures with reconstructive surgical options like skin flap, skin grafting, etc. in patients attending OPD after healing of burns.
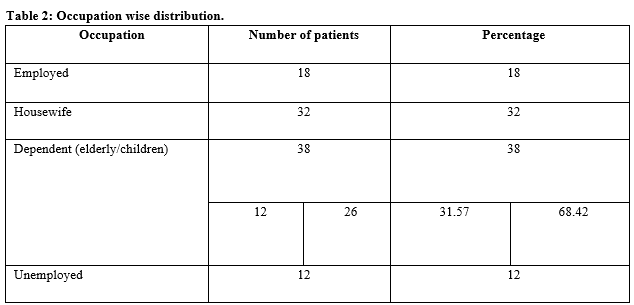
Methods: A prospective observational analysis was conducted, patients were analyzed and assessed with the help of a preformed questionnaire. Throughout this period a number of characteristics were evaluated on attending for an outpatient department like sex, age, social status, skin color, site, causes of burn, types of post-burn complications, psychological and social effects of burn on the patient, etc.
Results: Thermal burn (84%) is the most common cause of burns. Post-burn complications were most commonly seen in females of age group 15-30 years (77.27%), while it is more common in males of age group 30-45 years (52.63%). Post-burn complications were more common in the rural population of the low socio-economic group (61%).
Conclusion: Burns is a major concern for society and poses many psychiatric, social , aesthetic, and functional problems. The best approach is to avoid /prevent burns and when occurs, then it should be dealt with the utmost care and a holistic approach with proper concealing and rehabilitation is needed for these patients.
Downloads
References
Van Loey NE, Van Son MJ. Psychopathology and psychological problems in patients with burn scars. Am J Clin Dermatol. 2003;4(4):245-272. doi: 10.2165/00128071-200304040-00004.
Tucker P. Psychosocial problems among adult burn victims. Burns Incl Therm Inj. 1987;13(1):7-14. doi: 10.1016/0305-4179(87)90249-x.
Dyster-Aas J, Willebrand M, Wikehult B, Gerdin B, Ekselius L. Major depression and posttraumatic stress disorder symptoms following severe burn injury in relation to lifetime psychiatric morbidity. J Trauma. 2008;64(5):1349-1356. doi: 10.1097/TA.0b013e318047e005.
Bell PL, Gabriel V. Evidence based review for the treatment of post-burn pruritus. J Burn Care Res. 2009;30(1):55-61. doi: 10.1097/BCR.0b013e318191fd95.
Goel A, Shrivastava P. Post-burn scars and scar contractures. Indian J Plast Surg. 2010;43(Suppl):S63-S71. doi: 10.4103/0970-0358.70724.
Tyack ZF, Ziviani J. What influences the functional outcome of children at 6 months post-burn? Burns. 2003;29(5):433-444. doi: 10.1097/00004630-199909000-00007.
Davidson TN, Bowden ML, Tholen D, James MH, Feller I. Social support and post-burn adjustment. Arch Phys Med Rehabil. 1981;62(6):274-278.
Cowan AC, Stegink-Jansen CW. Rehabilitation of hand burn injuries: Current updates. Injury. 2013;44(3):391-396. doi: 10.1016/j.injury.2013.01.015.
Shakirov BM. Evaluation of different surgical techniques used for correction of post-burn contracture of foot and ankle. Ann Burns Fire Disasters. 2010;23(3):137-143.
Karki D, Mehta N, Narayan RP. Post-burn axillary contracture: A therapeutic challenge. Indian J Plastic Surgery. 2014;47(3):375-380. doi: 10.4103/0970-0358.146594.
Ndiaye L, Sankale AA, Ndiaye A, Foba ML, Coulibaly NF. Management of axillary burn contracture: A summary of 67 cases. Burns Open. 2018;2(3):109-113. doi: 10.1016/j.burnso.2018.06.003.
Beck B, Kumaran S, Nambi GI, Paul MK, Gupta AK, Dhanaraj P. A Clinical Study of Post Burn Breast Reconstruction. Indian J Burns. 2009;17(1):26-33.
Shahida F, Ismailb M, Khana S. Assessment of quality of life in post burn survivors: A cross-sectional single-center first validation study from Pakistan. Burns Open. 2018;2(1):35-42.
Agbenorku P, Aboah K, Akpaloo J, Amankwa R, Farhat B, Turkson E, et al. Epidemiological studies of burn patients in a burn center in Ghana: any clues for prevention. Burns Trauma. 2016;4:21. doi: 10.1186/s41038-016-0041-0.
Ibrahim A, Asuku M, Dahiru T. Burn prevention and first aid knowledge: A focus on adolescents in Zaria. Afr J Trauma. 2014:3(1):11-16. doi: 10.4103/1597-1112.139449.
Malik P, Garg R, Sharma KC, Jangid P, Gulia A. Quality of life in burn injury patients. Delhi Psychiatry J. 2012;15(2):308-315.
Chakraborty S, Bisoi S, Chattopadhyay D, Mishra R, Bhattacharya N, Biswas B. A study on demographic and profile of burn patients in an apex institute of west Bengal. Indian J Public Health. 2010;54(1):27-29. doi: 10.4103/0019-557X.70545.
Ganesamoni S, Kate V, Sadasivan J. Epidemiology of hospitalized burn patients in a tertiary care hospital in South India. Burns. 2010;36(3):422-429. doi: 10.1016/j.burns.2009.06.212.
Macharia LM. The Prevalence Of Depression Among Patients With Burns Admitted At Kenyatta National Hospital (Doctoral dissertation, University of Nairobi).
Tripathee S, Basnet SJ. Epidemiology of burn injuries in Nepal: a systemic review. Burns Trauma. 2017;5(1). doi: 10.1186/s41038-017-0075-y.
El-Maghawry HA, El Nem W, Sherif N, Hagag SA. An interventional study to decrease healthcare associated burn wound infections in the burn unit of Al Ahrar Hospital in Zagazig city, Sharkia Governorate. Int J Curr Microbiol Appp Sci. 2016;5(3):566-578. doi: 10.20546/ijcmas.2016.503.066.
Manzoor A, Khan AW, Gania AM, Suhaff AA, Baidya K. Comorbid Psychiatric Disorders in Burn patients -A Tertiary care Hospital Based study. Int J Inform Res Rev. 2016;3(5):2310-2314.
Ashfaq A, Lashari UG, Saleem S, Naveed S, Meraj H, Waqas A. Exploring symptoms of post-traumatic stress disorders and perceived social support among patients with burn injury. Cureus. 2018;10(5). doi: 10.7759/cureus.2669.
Buriro F, Nizam M, Bux AR. Success and Failures and Problems in the Management of Post Burn Contractures. doi: 10.13140/ RG.2.2.30069.58087.
Schneider JC, Holavanahalli R, Helm P, Goldstein R, Kowalske K. Contractures in burn injury: defining the problem. J Burn Care Res. 2006;27(4):508-514. doi: 10.1097/01.BCR.0000225994.75744.9D.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


















 Therapoid
Therapoid

