Clinicopathological features of Pseudocyst Pancreas and its Management: A Prospective and Retrospective Study
Abstract
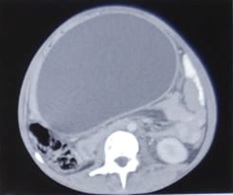
Background: Revised Atlanta Classification has veered a change in our understanding of pseudocyst pancreas which mandates renewed inquiry into pseudocysts defined as per new criteria. The present study provides an overview of experience with Pseudocyst Pancreas for over a decade.
Methodology: 100 cases of pseudocysts diagnosed over the last 10 years at GMC, Bhopal, conforming to the present definition were reviewed. Cysts with the inhomogeneous collection, debris, necrosis, or any other non-liquid component, specifically in those diagnosed before 2012 were excluded. Relevant data were analyzed.
Results: The majority were male (85%) in the age group of 40-50 years with alcohol-induced chronic pancreatitis (77%) being the most frequent etiology. Abdominal pain (40%), lump (30%), and abdominal tenderness (59%) were common at presentation. 58% were in the Head of the pancreas, 29% in the Neck and Body, and 13% in the Tail and surrounding areas. Mean cyst diameter was 8.6cm and volume 252cc. 85% were managed surgically and 40% of those managed conservatively also needed surgical intervention eventually due to complications. History of chronic alcoholic pancreatitis, the large size of the cyst (≥6cm and ≥60cc), and communication with the main pancreatic duct were highly predictive of surgical intervention.
Conclusion: Radiological characteristics along with the clinical picture may suggest appropriate intervention. Surgery remains the principal modality of treatment, with high success rates.
Downloads
References
Costa P, Rego A, Araujo-Filho I. Pancreatic cystic lesions: classification, diagnosis and treatment. Int Surg J. 2016;3(2):443-451. doi: 10.18203/2349-2902.isj20160666.
Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, et al. Classification of acute pancreatitis—2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62(1):102-111. doi: 10.1136/gutjnl-2012-302779.
Tan J, Zhou L, Cao R, Zhang G. Identification of risk factors for pancreatic pseudocysts formation, intervention and recurrence: a 15-year retrospective analysis in a tertiary hospital in China. BMC Gastroenterology. 2018;18(1)1-9. doi: 10.1186/s12876-018-0874-z.
Yip H, Teoh A. Endoscopic Management of Peri-Pancreatic Fluid Collections. Gut Liver. 2017;11(5):604-611. doi: 10.5009/gnl16178.
Usatoff V, Brancatisano R, Williamson R. Operative treatment of pseudocysts in patients with chronic pancreatitis. Brit J Surg. 2000;87(11):1494-1499. doi: 10.1046/j.1365-2168.2000.01560.x.
Aghdassi AA, Mayerle J, Kraft M, Sielenkämper AW, Heidecke CD, Lerch MM. Pancreatic pseudocysts – when and how to treat?. HPB. 2006;8(6):432-441. doi: 10.1080/13651820600748012.
Habashi S, Draganov P. Pancreatic pseudocyst. World J Gastroenterol. 2009;15(1):38. doi: 10.3748/wjg.15.38.
Guardado-Bermúdez F, Azuara-Turrubiates AJ, Ardisson-Zamora FJ, Guerrero-Silva LA, Villanueva-Rodríguez E, Gómez-de Leija NA, et al. Pancreatic pseudocyst. Case report and literature review. Cir Cir. 2014;82(4):425-431.
Samokhvalov AV, Rehm J, Roerecke M. Alcohol consumption as a risk factor for acute and chronic pancreatitis: a systematic review and a series of meta-analyses. EBioMedicine. 2015;2(12):1996-2002. doi: 10.1016/j.ebiom.2015.11.023.
Aghdassi A, Mayerle J, Kraft M, Sielenkämper AW, Heidecke CD, Lerch MM. Diagnosis and treatment of pancreatic pseudocysts in chronic pancreatitis. Pancreas. 2008;36(2):105-112. doi: 10.1097/MPA.0b013e31815a8887.
Farias GFA, Bernardo WM, De Moura DTH, et al. Endoscopic versus surgical treatment for pancreatic pseudocysts: Systematic review and meta-analysis. Med (Baltimore). 2019;98(8):e14255. doi: 10.1097/MD.0000000000014255.
Almaihan A, Matar A, Murshid E, Al-Ostaz S, Shebly A, Miftah M, et al. Conservative management versus surgical drainage in pancreatic pseudocyst. Int Surg J. 2018;5(7):2383. doi: 10.18203/2349-2902.isj20182438.
Ito K, Perez A, Ito H, Whang EE. Pancreatic pseudocysts: is delayed surgical intervention associated with adverse outcomes. J Gastrointest Surg. 2007;11(10):1317–1321. doi:10.1007/s11605-007-0237-5.
Tan JH, Zhou L, Cao RC, Zhang GW. Identification of risk factors for pancreatic pseudocysts formation, intervention and recurrence: a 15-year retrospective analysis in a tertiary hospital in China. BMC Gastroenterology. 2018;18(1):1-9. doi: 10.1186/s12876-018-0874-z.
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


















 Therapoid
Therapoid

