The relation between pelvic trauma (fractured pelvis) with posterior urethral distraction injury associated with erectile dysfunction
Abstract
Background: The aim was to study the relation between posterior urethral distraction injury due to pelvic trauma (fractured pelvis) with erectile dysfunction and to do the clinical assessment of Erectile dysfunction by penile Doppler study for assessment of peak flow velocity.
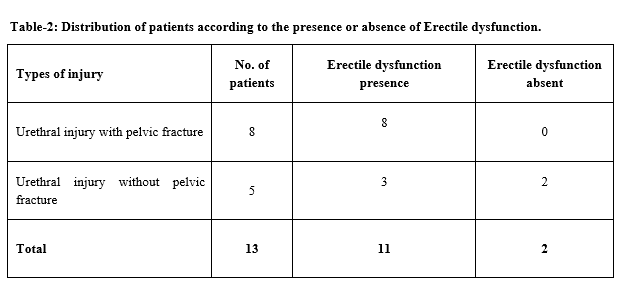
Material and Methods: Total number of cases included in the study was 13, out of which 5 patients belonged to young (<30 years) age group, 5 patients belonged to middle (30-50 years) age group and 3 patients belonged to old age group. Out of the total 13 patients, 8 patients had pelvic fracture associated with urethral injury and 5 patients had traumatic urethral stricture without pelvic fracture.
Results: Out of 8 patients of pelvic fracture with urethral injury, all 8 developed erectile dysfunction after trauma. While among 5 patients of traumatic urethral stricture without pelvic fracture, 3 patients developed erectile dysfunction after trauma. While in traumatic urethral injury without pelvic fracture, amongst 3 patients who had erectile dysfunction, 2 patients had reduced flow on penile Doppler ultrasound and were classified as vascular erectile dysfunction while 1 patient was having a normal flow on penile Doppler ultrasound and was classified as neurogenic/psychological erectile dysfunction.
Conclusion: Pelvic fracture associated urethral injury has a high incidence of erectile dysfunction. Vascular erectile dysfunction in such patients is more common than neurogenic/psychological erectile dysfunction. And postoperatively (urethroplasty), there is no significant decrease in penile colour doppler vascularity in such patients.
Downloads
References
Dalinka MK, Arger P, Coleman B. CT in pelvic trauma. Orthop Clin North Am. 1985;16(3):471-480.
Mundy AR. Pelvic fracture injuries of the posterior urethra. World J Urol. 1999;17(2):90-95.
Bjurlin MA, Fantus RJ, Mellett MM, Goble SM. Genitourinary injuries in pelvic fracture morbidity and mortality using the National Trauma Data Bank. J Traum Acute Care Surg. 2009;67(5):1033-1039.
Jequier S, jequier JC. Reliability of voidind cystourethrography to detect reflux. AJR Am J Rontgenol. 1989;153(4):807-810.
Jordan GH, McCammon KA. Surgery of the penis and urethra. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CP, eds. Campbell’s Urology, 10th ed, Philadelphia, Pa: Elsevier Saunders;2012:3012-3064.
Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA. Campbell-Walsh urology: expert consult premium edition: enhanced online features and print, 4-volume set. Elsevier Health Sciences; 2011 Aug 25.
Brooks JD. Anatomy of the lower urinary tract and male genitalia. Campbell-walsh urology. 2007.
Andrich DE, Day AC, Mundy AR. Proposed mechanisms of lower urinary tract injury in fractures of the pelvic ring. BJU Int. 2007;100(3):567-573.
Lawson CM, Daley BJ, Ormsby CB, Enderson B. Missed injuries in the era of the trauma scan. J Trauma Acute Care Surg. 2011;70(2):452-458.
Mouraviev VB, Santucci RA. Cadaveric anatomy of pelvic fracture urethral distraction injury: most injuries are distal to the external urinary sphincter. J Urol. 2005;173(3):869-872.
Latini JM, McAninch JW, Brandes SB, Chung JY, Rosenstein D. SIU/ICUD consultation on urethral strictures: epidemiology, etiology, anatomy, and nomenclature of urethral stenoses, strictures, and pelvic fracture urethral disruption injuries. Urol. 2014;83(3):S1-S7.
Dalal AK, Sinha TP, Mohanty D. Pelvic fracture and urogenital injuries. J Orthoped, Traumatol Rehabilit. 2014;7(1):29.
Wright JL, Nathens AB, Rivara FP, MacKenzie EJ, Wessells H. Specific fracture configurations predict sexual and excretory dysfunction in men and women 1 year after pelvic fracture. J Urol. 2006;176(4):1540-1545.
Pariser JJ, Pearce SM, Patel SG, Bales GT. National patterns of urethral evaluation and risk factors for urethral injury in patients with penile fracture. Urol. 2015;86(1):181-186.
Dixon CM, Saunder WB. Diagnosis and acute management of posterior urethral disruptions. Traumatic and reconstructive urology. Philadelphia: WB Saunders. 1996:347-355.
Feng C, Xu YM, Yu JJ, Fei XF, Chen L. Risk factors for erectile dysfunction in patients with urethral strictures secondary to blunt trauma. J Sex Med. 2008;5(11):2656-2661.
Shenfeld OZ, Kiselgorf D, Gofrit ON, Verstandig AG, Landau EH, Pode D. The incidence and causes of erectile dysfunction after pelvic fractures associated with posterior urethral disruption. J Urol. 2003;169(6):2173-2176.
El-Assmy A, Harraz AM, Benhassan M, Fouda M, Gaber H, Nabeeh A, et al. Erectile dysfunction post-perineal anastomotic urethroplasty for traumatic urethral injuries: analysis of incidence and possibility of recovery. Int Urol Nephrol. 2015;47(5):797-802.
Anger JT, Sherman ND, Dielubanza E, Webster GD. Erectile function after posterior urethroplasty for pelvic fracture‐urethral distraction defect injuries. BJU Int. 2009;104(8):1126-1129.
Koraitim MM. Predictors of erectile dysfunction post pelvic fracture urethral injuries: a multivariate analysis. Urol. 2013;81(5):1081-1085.
Guan Y, Wendong S, Zhao S, Liu T, Liu Y, Zhang X, et al. The vascular and neurogenic factors associated with erectile dysfunction in patients after pelvic fractures. Int Braz J Urol. 2015;41(5):959-966.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


















 Therapoid
Therapoid

