Non-invasive preoperative assessment of ureteral stone impaction using peri-calculus ureteral thickness on Non-Contrast CT (NCCT) scan: A prospective Study
Abstract
Background: Ureteral stone can be measured on the NCCT scan as peri-calculus ureteral thickness. If this depicts significant calculus impaction, the patient could be counseled regarding intra-operative risk and incomplete stone clearance. The present study was planned to evaluate the use of NCCT in patients with ureterolithiasis for the prediction of a favorable clinical outcome.
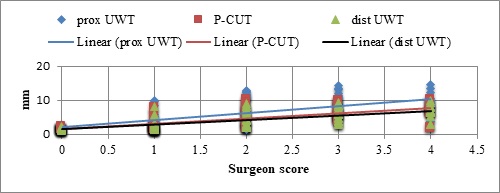
Materials and methods: Patients who underwent ureterorenoscopy for ureteric calculus with pre-operative NCCT scan were included and intraoperative data were recorded. Operating surgeons were blinded for proximal ureteric wall thickness (p-UWT), peri-calculus ureteric wall thickness (p-CUT), and distal ureteric wall thickness (d-UWT) values. The guidewire was negotiated before each URS. Stone was considered impacted if guidewire could not be negotiated in 2 attempts. Intra-operative stone impaction score (SIS) assigned on a scale of 0 (dislodged spontaneously), 1 (dislodged with saline pressure), 2 (dislodged after lithotripsy), 3 (fragments impacted in edema) and 4 (open). Intra-operative findings were correlated to preoperative NCCT measurements of ureteral thickness. Other variables like duration of symptoms, hydronephrosis, stone size in the longest dimension, and stone location were also recorded.
Results: Of total patients 108 patients, 70 patients had non-impacted calculus and 38 patients had impacted calculus. Patients with an impacted calculus had significantly higher p-UWT (9.76 ±3.11mm), p-CUT (6.82±2.57mm), and d-UWT (6.26±2.28mm) as compared to non-impacted. There was a positive correlation in SIS with p-UWT, p-CUT, and p-DWT in both impacted and non-impacted groups.
Conclusion: Pre-operative ureteric wall thickness in proximal, peri, and distal to calculus can predict intraoperative risk and impaction of calculus.
Downloads
References
D’Addessi A, Francesco Bassi PF. Ureterorenoscopy: Avoiding and Managing Complications. Urol Int. 2011;87(3):251-259. doi: https://doi.org/10.1159/000329286.
Cho SY, Na W, Lee SW, Cho MC, Oh JJ, Lee S, et al. Medical expulsive therapy for ureter stone using naftopidil : A multicenter, randomized, double-blind, and placebo-controlled trial. PLoS ONE. 2017;12(4):e0174962. doi: https://doi.org/10.1371/journal.pone.0174962.
Protogerou V. Management and follow-up of impacted ureteral stones. Urol Int. 2003;70(4):269-272. doi: https://doi.org/10.1159/000070133.
Elganainy E, Hameed DA, Elgammal MA, Abd-elsayed AA, Shalaby M. Experience with impacted upper ureteral Stones ; should we abandon using semirigid ureteroscopes and pneumatic lithoclast ?. Int Arch Med. 2009;2(1):13. doi: https://doi.org/10.1186/1755-7682-2-13.
Nagae H. Endoscopic features of impacted ureteral stones. J Urol. 2004;171(1):89-91. doi: https://doi.org/10.1097/01.ju.0000100960.08768.81.
Takahashi N, Ernst RD, Goldman SM, Benson GS, Sandier CM. Ureterolithiasis : can clinical outcome be predicted with unenhanced helical CT? Radiol. 1998;208(1):97-102. doi: https://doi.org/10.1148/radiology.208.1.9646798.
Feroze S, Singh B, Gojwari T, Manjeet S, Athar B, Hamid H. Role of non-contrast spiral computerized tomography in acute ureteric colic. Indian J Urol. 2007;23(2):119-121. doi: https://doi.org/10.4103/0970-1591.32059.
Shokeir AA, El-diasty T, Eassa W, Mosbah A, El-Ghar MA, Mansour O, et al. Diagnosis of ureteral obstruction in patients with compromised renal function: the role of noninvasive imaging modalities. J Urol. 2004;171(6 Part 1):2303-2306. doi: https://doi.org/10.1097/01.ju.0000124928.69055.10.
Smith RC, Verga M, McCarthy SM, Rosenfield AT. Diagnosis of acute flank pain: value of unenhanced helical CT. Am J Roentgenol. 1996;166(5):97-101. doi: https://doi.org/10.2214/ajr.166.1.8571915.
Elibol O, Safak KY, Buz A, Eryildirim B, Erdem K, Sarica K. Radiological noninvasive assessment of ureteral stone impaction into the ureteric wall : A critical evaluation with objective radiological parameters. Investig Clin Urol. 2017;58(5):339-345. doi: http://dx.doi.org/10.4111/icu.2017.58.5.339.
Mugiya S, Ito T, Maruyama S, Hadano S, Nagae H. Endoscopic features of impacted ureteral stones. J Urol. 2004;171(1):89-91. doi: https://doi.org/10.1097/01.ju.0000100960.08768.81.
Chandhoke R, Bamberger JN, Gallante B, Atallah W, Gupta M. Pericalculus ureteral thickness on computed tomography predicts stone impaction at the time of surgery: a prospective study. J Endourol. 2020;34(1):107-111. doi: http://doi.org/10.1089/end.2019.0449.
Latif AMA. Ureteroscopic holmium lasertripsy for treatment of impafted ureteral calculi. Af J Urol. 2007;13(4):262-266. Available at https://www.ajol.info/index.php/aju/article/view/8213.
Legemate JD, Wijnstok NJ, Matsuda T, Strijbos W, Erdogru T, Roth B, et al. Characteristics and outcomes of ureteroscopic treatment in 2650 patients with impacted ureteral stones. World J Urol. 2017;35(10):1497-1506. doi: https://doi.org/10.1007/s00345-017-2028-2.
Leijte JAP, Oddens JR, Lock TMTW. Holmium Laser Lithotripsy for Ureteric Calculi : Predictive Factors for Complications and Success. J Endourol. 2008;22(2):10-13. doi: https://doi.org/10.1089/end.2007.0299.
Seitz C, Tanovic E, Kikic Z, Fajkovic H. Impact of stone size, location, composition, impaction, and hydronephrosis on the efficacy of Holmium: YAG-Laser Uretero lithotripsy. Europe Urol. 2007;52(6):1751-1759. doi: https://doi.org/10.1016/j.eururo.2007.04.029.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


















 Therapoid
Therapoid

