A study to isolate various bacteria causing osteomyelitis in a tertiary health care setup
Abstract
Introduction: Osteomyelitis (OM), an inflammation of bone or bone marrow caused by various infectious agents, can cause any age. With this, a study was taken to isolate various bacterial etiological agents that cause OM.
Material and Methods: It was a laboratory-based study, conducted in the Department of Microbiology, GSL Medical College from June to Nov 2019. Individuals of all ages, both genders, clinically, radiologically confirmed cases of OM were included in the study. Bone, tissue, and swabs collected with utmost sterile precautions were considered, cultured as per the standard methods. Antibiotic susceptibility test was performed for various pathogenic isolates using Kirby Bauer disc diffusion method; P<0.05 was considered statistically significant.
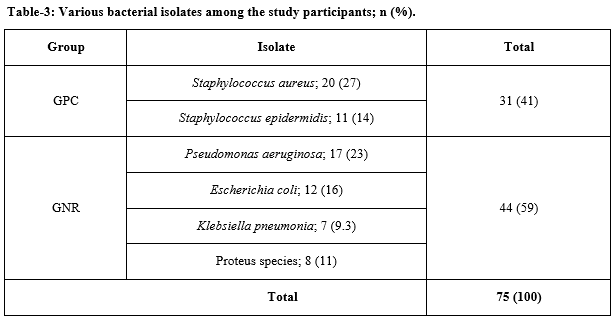
Results: During the study period a total of 72 samples were collected, 61 were culture positive (CP). Age-wise, maximum (18%) CP results were identified in 31-40 years of age group followed by 41-50 years group. Gram-negative rods were isolated maximum (59%) and Staph. aureus was the maximum isolate.
Conclusion: OM can occur at any age and there is no gender difference. Staph. aureus was a common isolate followed by Pseudomonas.
Downloads
References
del Pozo EG, Collazos J, Cartón JA, Camporro D, Asensi V. Bacterial osteomyelitis: microbiological, clinical, therapeutic, and evolutive characteristics of 344 episodes. Revista Española de Quimioterapia. 2018;31(3):217-225.
Hogan A, Heppert VG, Suda AJ. Osteomyelitis. Arch Orthop Trauma Surg. 2013;133(9):1183-1196. doi: https://doi.org/10.1007/s00402-013-1785-7.
Radcliffe G. Osteomyelitis: a historical and basic sciences review. Orthop Trauma. 2015;29(4):243-252. doi: https://doi.org/10.1016/j.mporth.2015.02.002.
Carvalho VC, Oliveira PR, Dal-Paz K, Paula AP, Félix Cda S, Lima AL. Gram-negative osteomyelitis: Clinical and microbiological profile. Braz J Infect Dis. 2012;16(1):63-67. doi: https://doi.org/10.1016/S1413-8670(12)70276-3.
Abid AS, Ehan AH, Yonis AR. Epidemiological and bacteriological study of chronic osteomyelitis. Tikrit. Med J. 2008;14(1):59-62.
Dartnell J, Ramachandran M, Katchburian M. Haematogenous acute and subacute paediatric osteomyelitis: a systematic review of the literature. J Bone Joint Surg Br. 2012;94(5):584-595. doi: https://doi.org/10.1302/0301-620x.94b5.28523.
Vazquez M. Osteomyelitis in children. Curr Opin Pediatr. 2002;14(1):112-115. doi: https://doi.org/10.1097/00008480-200202000-00020.
Shettigar S, Shenoy S, Bhat S, Rao P. Microbiological Profile of Deep Tissue and Bone Tissue in Diabetic Foot Osteomyelitis. J of Clil and Diagic Rese. 2018;12(6):DC20-DC22. doi: https://doi.org/10.7860/JCDR/2018/35462.11597.
Chandra TJ, Lakshmi Prasanna, AV Rao. A study on isolation and identification of nosocomial infections causing bacteria on mobile phones of health care workers. Calicut Med J. 2011;9(1):e2.
Chihara S, Segreti J. Osteomyelitis. Dis Mon. 2010;56(1):5–31. doi: https://doi.org/10.1016/j.disamonth.2009.07.001.
Tulner SAF, Schaap GR, Strackee SD, Besselaar PP, Luitse JSK, Marti RK. Long-term results of multiple-stage treatment for posttraumatic osteomyelitis of the tibia. J Trauma. 2004;56(3):633-642. doi: https://doi.org/10.1097/01.ta.0000112327.50235.0a.
Solagberu BA, Duze AT, Ofoegbu C P, Adekanye AO, Odelowo EO. Surgical morbidity and mortality pattern in the accident and emergency room—a preliminary report. Afr J Med Med Sci. 2000;29(3):315-318.
Tummala VS, Surapaneni SB, Pigilam S. Bacteriological study of orthopaedic infections. Int J Orthopaed. 2017;3(2):90-92. doi: https://doi.org/10.22271/ortho.2017.v3.i2b.17.
Neeharika B, Vinod R, Rakesh G. A study of aerobic bacterial profile and their antibiogram in patients with chronic osteomyelitis with special references to staphylococcus aureus. Ind J Microbiol Res. 2019;6(4):350-354. doi: http://doi.org/10.18231/j.ijmr.2019.074.
Wadekar DM, Anuradha K, Venkatesha D. Chronic osteomyelitis: Aetiology and antibiotic susceptibility pattern. Int J Recent Trends Sci Technol. 2014;9(3):337-340.
Vemu L, Sudhaharan S, Mamidi N, Chavali P. Need for appropriate specimen for microbiology diagnosis of chronic osteomyelitis. J Lab Physicians. 2018;10(1):21-25. doi: https://doi.org/10.4103/jlp.jlp_14_17.
Kao HC, Huang YC, Chiu CH, Chang LY, Lee ZL, Chung PW et al. Acute hematogenous osteomyelitis and septic arthritis in children. J Microbiol Immunol Infect. 2003;36:260-265.
Carek PJ, Dickerson LM, Sack JL. Diagnosis and management of osteomyelitis. Am Fam Physician. 2002;63(12):2413-2420.
Gavilán MG, López JB, Artola BS. Peculiarities of osteoarticular infections in children. Best Pract Res Clin Rheumatol. 1999;13(1):77-94. doi: http://doi.org/10.1053/berh.1999.0007.
Thanni LOA, Kehinde OA. Trauma at a Nigerian teaching hospital: pattern and documentation of presentation. African Health Sci. 2006;6(2):104-107.
Prieto-Pérez L, Pérez-Tanoira R, Petkova-Saiz E, Pérez-Jorge C, Lopez-Rodthop. Osteomyelitis: a descriptive study. Clin Orthop Surg. 2014;6(1):20-25. doi: https://doi.org/10.4055/cios.2014.6.1.20.
Smith IM, Austin OMB, Batchelor AG. The treatment of chronic osteomyelitis: a 10-year audit. J Plast Reconstr Aesthet Surg. 2006;59(1):11-15. doi: https://doi.org/10.1016/j.bjps.2005.07.002.
Priest DH, Peacock JE jr, studies on haematogenous vertebral osteomyelitis due to Staphylococcus aureus in adults South Med. J. 2006;98(9):854-862. doi: https://doi.org/10.1097/01.smj.0000168666.98129.33.
Pappu AK, Sinha A, Johnson A. Microbiological profile of diabetic foot ulcer. Calicut Med J. 2011;9(3):e1-e4.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


















 Therapoid
Therapoid

