Normal Saline versus Honey Dressing in the Preparation for Skin Grafting
Abstract
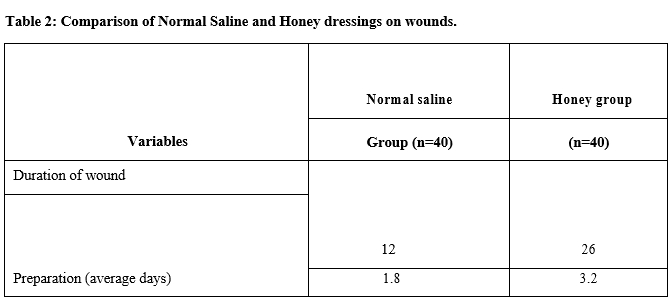
Objective: To compare the continuously wet normal saline and honey gauze dressings in terms of days required for wound preparation for skin grafting and graft take.
Material and Methods: The present study was a Quasi-experimental which was conducted in the Department of General Surgery, GEMS, Ragolu, Srikakulam Andhra Pradesh from January to November 2019.
Methodology: Eighty wounds with small patches of slough and pale granulation tissue requiring preparation for skin grafting were included and divided into two groups by simple random sampling. Wounds requiring mechanical debridement or grossly infected wounds, diabetics, and patients with age > 60 years, Hb <10 g/dl, and serum albumin level ≤ 3 g/dl were excluded. Time for wound preparation in days was noted. Split thickness skin grafts meshed to 1-1.5 were applied. The largest area of graft loss in both wounds was measured in the two largest dimensions and noted in cm2. This was the endpoint of the study.
Results: Average time for preparation in the saline group was 10 days whereas the average time in the honey group was 27 days. The average area of graft loss in the saline group and honey group was 2 cm2 and 3 cm2 respectively.
Conclusion: Normal saline dressing is a hyperosmolar physiological dressing and prepares the wound faster than honey dressing at a low cost with quite satisfactory graft take.
Downloads
References
Christian EP, Jeffrey JP, Peter R. Skin Grafts. In: Ste-phen JM. Plastic Surgery General Principles. 2nd ed. Philadelphia: Saunders Elsevier; 2006; 299.
Robert DG, Thomas AM. Wound care. In: Charles HT, Robert WB, Sherrell JA, Scott PB, Geoffrey CG, Scott
LS. Grab and Smith’s Plastic Surgery. 6th ed. Philadel-phia: Lippincot William and Wilkins; 2007; 27.
Bohdan P, Tobias H, Elof E. Wound management. In: Bahman G, Elof E, John AP. Plastic Surgery. 1st ed. Philadelphia: Saunders Elsevier; 2009; 29.
Bohdan P, Tobias H, Elof E. Wound management. In: Bahman G, Elof E, John AP. Plastic Surgery. 1st ed. Philadelphia: Saunders Elsevier; 2009; 31.
Myers BA. Wound Management principles and prac-tice. New Jersey(NJ) : Pearson Education Inc; 2004: 80-81.
Archer HG, Barnett S, Irving S, Middleton KR. Seal DV. A controlled model of moist wound healing: Com-parison between semipermeable film, antiseptics and sugar paste. J Exp Patho 1990; 71: 155-170.
Gajiwala k, Gajiwala AL. Evaluation of Lypholized, gamma irradiated amnion as a biological dressing. Cell Tissue bank 2004; 5: 73-80.
Gore MA, Akolekar D. Evaluation of Banana leaf dres-sing for partial thickness burn wounds. Burns 2003; 29: 487-92.
Ayodeji AS, Innocent OI, Olatunde OO. A comparison of the effect of chlorhexidine, Tap water and Normal saline on wound healing. Int J Morphol 2006; 24: 673-676.
Lim JK, Saliba L, Smith MJ, McTavish J, Raine C,
Curtain P. Normal Saline wound dressing─ is it really normal? Br J Plast Surg 2000; 53: 42-45.
Owen AM, Lesley AS, Fiona C, Kate S, Henery JM, Andrew RM. Systematic review of the use of honey as a wound dressing. BMC Complimentary and Alter-native Medicine 2001; 1: 2.
Nagra ZM, Fayyaz GQ, Asim M. Honey dressings: Experience at department of plastic surgery and burns allied hospital, Faisalabad. Prof Med J 2002; 9: 246-51.
Abdulrazzak M, Tahir SM, Imdad AK, Ghulam Ali M. Therapeutic effects of honey versus silver sulphadiazine in the management of burn injuries. J Liaquat Uni Med Health Sci 2005; 4: 100-4.
Ovington LG, Hanging wet to dry dressing out to dry, Advances in skin and wound care. The journal for Pre-vention and Healing 2002; 15: 79-84.
Alex S, Ian LV, Ernest KM. Grafts. In: Bahman G, Elof E, John AP. Plastic Surgery.1st ed. Philadelphia: Saun-
ders Elsevier; 2009: 97.
Timothy G. Plastic and reconstructive surgery. In: Nor-man SW, Christopher JKB, Ronan POC. Bailey and Love’s Short Practice of Surgery. 25th ed. Arnold: Lon-don; 2008: 401.
Svensio T, Pomahac F, Yao J. Accelerated healing of full thickness skin wounds in a wet environment. Plast Recons Surg 2000; 106: 602-614.
Bardely M, Cullum N, Nelson EA. Systematic reviews of wound care management: Dressings and topical agents used in the healing of chronic wounds. Health Technol Assess 1999; 3: 1-35.
Copper RA, Molan P, Harding KG. Antibacterial acti-vity of honey against strains of Staphylococcus aureus from infected wounds. J Ray Soc Med 1999; 92: 283-85.
Cooper RA, Molan PC. The use of honey as an anti-septic in managing Pseudomonas infection. J wound Care 1999; 8: 161-4.
Karayil S, Deshpande SD, Koppikar GV. Effect of ho-ney on multi-drug resistant organisms and its syner-gistic action with three common antibiotics. J Postgrad Med 1998; 44: 93-6.
Sibbald R, Williamson GD, Orsted H, Campbell LK, Keast D, Krasner D et al. Preparing the wound bed─ debridement, bacterial balance and moisture balance. Ostomy/ wound management 2000; 46: 14-35.
Whaley S. Tap water or normal saline for cleansing tra-umatic wounds? British J Community Nursing 2004; 9: 471-8.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


















 Therapoid
Therapoid

