A retrospective cohort study of diabetic foot disease during the covid pandemic in a tertiary care hospital in Kerala
Mohandas P.1, Vasu Keloth A.2*, G Krishnan D.3, Rahman N.4
DOI: https://doi.org/10.17511/ijoso.2021.i04.01
1 P.G. Mohandas, Professor, Department of General Surgery, KMCT Medical College, Kozhikode, Kerala, India.
2* Anukesh Vasu Keloth, Assistant Professor, Department of General Surgery, KMCT Medical College, Kozhikode, Kerala, India.
3 Divya G Krishnan, Associate Professor, Department of Pharmacology, KMCT Medical College, Kozhikode, Kerala, India.
4 Neema Rahman, Junior Resident, Department of General Surgery, KMCT Medical College, Kozhikode, Kerala, India.
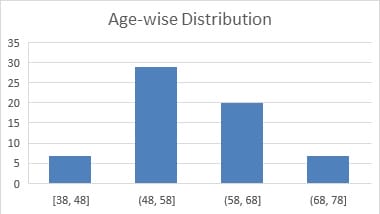
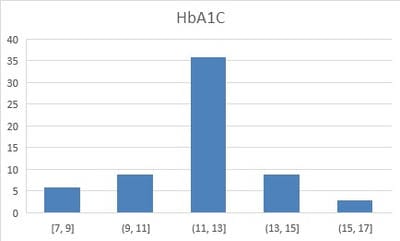
Introduction: Diabetes affects 88 million people in south-east Asia with a regional prevalence of 8.8%, and of them, 77 million live in India. Diabetic Foot Disease is an important complication that accounts for significant morbidity and mortality in a diabetic individual. Aim: This study was conducted to study the presentation stage of diabetic foot disease during the pandemic period as seen at a tertiary care hospital in North Kerala. Methods: This was a retrospective cohort study carried out on patients diagnosed with diabetic foot and admitted to the Department of Surgery of a tertiary care hospital in North Kerala during the study period of 6months from July 2020 to December 2020. A sample size of 63 was calculated. Data were collected from the case records of the patients, and the stages of presentation, relevant blood investigations, culture reports, radiological imaging and arterial doppler ultrasound findings were noted. Results: In this study, a total of 63 patients were included. Of the 63 patients, 51(80.9%) were males, and 12 (19.0%) were females with a male to female ratio of 4.25:1. The mean age of the patients was 57.74 years. In this study, as per the Wagner-Meggitt Classification of diabetic foot, the most common stage of presentation of diabetic foot encountered was Grade III (42.9%) followed by Grade IV (28.6%), Grade II (19.0%) and Grade V (9.5%). Conclusion: This is in part may be due to financial constraints of the patient's families due to lack of job, transportation difficulties, shortage of medicines, shutting down of small scale health care facilities and pharmacies, prolonged neglect of wounds, discontinuing of regular medications and poor home wound care which in turn are due to the frequent regional lockdowns as a result of the covid pandemic.
Keywords: Diabetic Foot Disease, Foot Ulcer, Wagner-Meggitt Classification
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of General Surgery, KMCT Medical College, Kozhikode, Kerala, India. Email: |
P.G. Mohandas, Anukesh Vasu Keloth, Divya G Krishnan, Neema Rahman, A retrospective cohort study of diabetic foot disease during the covid pandemic in a tertiary care hospital in Kerala. Surgical Rev Int J Surg Trauma Orthoped. 2021;7(4):78-84. Available From https://surgical.medresearch.in/index.php/ijoso/article/view/239 |


 ©
©