Laparoscopic Anterior 180° Partial Fundoplication - Indian Perspective
Biswabasu Das.1*, Sandeep Sahu.2, Radhakrishna Y.3, Bibhabasu Das.4
DOI: https://doi.org/10.17511/ijoso.2021.i03.01
1* Biswabasu Das, Mch, Department of Surgical Gastroenterology, Seven Hills Hospital, Vizag, Andhra Pradesh, India.
2 Sandeep Sahu, DNB, Department of Surgical Gastroenterology, Seven Hills Hospital, Vizag, Andhra Pradesh, India.
3 Radhakrishna Y, DM, Department of Gastroenterology, Radhakrishna Gastro Center, Vizag, Andhra Pradesh, India.
4 Bibhabasu Das, B Tech, Department of Mechanical Engineering, IIT Madras, Chennai, Tamil Nadu , India.
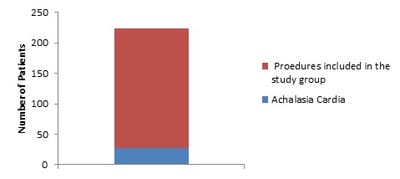
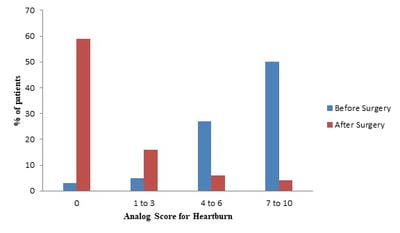
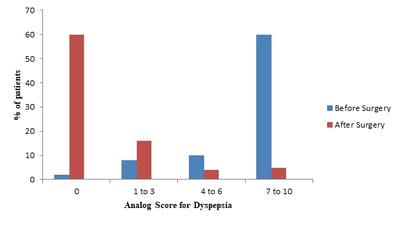
Aim: To evaluate Laparoscopic anterior 180° partial fundoplication for its good long-term relief for symptoms of gastroesophageal reflux disease and association with adverse effects. Methods: Study design: Prospectively evaluated case series. Settings: Tertiary care centers Patients: The clinical outcomes were determined for all patients who had undergone a laparoscopic anterior partial fundoplication by us between January 1, 2013 to March 31, 2021. Interventions: Clinical outcome, complications, and follow-up after laparoscopic anterior 180° partial fundoplication was obtained using a structured questionnaire. Results and Discussion: 228 procedures were performed. The outcome at 0 to 8 years (mean, 4 years) follow-up was determined for 195 patients. 1 death was linked to the laparoscopic procedure and 2 patients died during follow-up due to unrelated causes. For 186 patients (95%) with clinical outcome data at late follow-up, gastroesophageal reflux symptoms were significantly improved following surgery and were well controlled in 9 patients (4.5%). In a subset of 85 patients with more than 5 years of follow-up, relief of heartburn was found in 59 patients (69%). Incidence and severity of heartburn were reduced after surgery in 22 patients (26%), decreased dyspepsia in 80 patients (94%). Normal belching was preserved in 84 patients (99%) and almost all patients were able to eat normally. Conclusion: Laparoscopic anterior 180° partial fundoplication is an effective procedure for the surgical treatment of gastroesophageal reflux and is associated with a high rate of patient satisfaction at late follow-up. Compared to Nissen's fundoplication it is as good as control of recurrent reflux as well as reduced adverse effects. The patient goes home in 3-4 days. Hence we recommend it as the procedure of choice for reflux symptoms.
Keywords: Laparoscopic Anterior 180° Partial Fundoplication, Gastroesophageal Reflux Disease (GERD), Dyspepsia
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Mch, Department of Surgical Gastroenterology, Seven Hills Hospital, Vizag, Andhra Pradesh, India. Email: |
Das B, Sahu S, Radhakrishna Y, Das B. Laparoscopic Anterior 180° Partial Fundoplication - Indian Perspective. Surgical Rev Int J Surg Trauma Orthoped. 2021;7(3):36-43. Available From https://surgical.medresearch.in/index.php/ijoso/article/view/233 |


 ©
©