Functional outcome of minimally invasive plate osteosynthesis (MIPO) in proximal tibial fractures
Vora J.1, Shah J.2*, Vala G.3
DOI: https://doi.org/10.17511/ijoso.2020.i02.05
1 Jinesh Vora, Associate Professor, Department of Orthopaedics, C.U Shah Medical College and Hospital, Surendranagar, Gujarat, India.
2* Jay Shah, Postgraduate Student, Department of Orthopaedics, C.U Shah Medical College and Hospital, Surendranagar, Gujarat, India.
3 Gaurav Vala, Associate Professor, Department of Orthopaedics, C.U Shah Medical College and Hospital, Surendranagar, Gujarat, India.
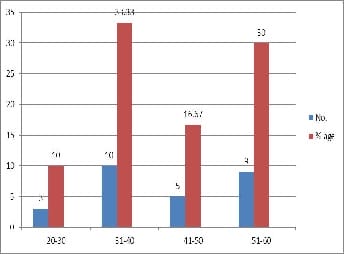
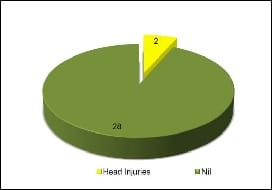
Introduction: This study is undertaken to evaluate the outcome of the MIPO technique in Proximal Tibial Condyle Fractures which is expected to provide a stable fixation with minimum exposure, early mobilization, fewer complications, and a better quality of life. Material and methods: Study design: Prospective cohort study carried out at C.U Shah Medical College. 30 cases of proximal tibia fractures (Schatzker type 1- VI) operated with the MIPO technique. Follow-up of these patients was done at 6 months and 9 months after surgery by using Sanders's 40-point functional scale. Results: There were 16 cases of Schatzker type I fractures, 5 cases of Type II, 4 cases of type III, 2 cases of type IV, 1 case of type V and 2 cases of type VI fractures. The healing process was determined by radiographically and functionally. Meantime to union was 17.6 weeks, with 50 % of fractures uniting in 14-16 weeks. Infection was observed in two cases (10%), two cases of collapse of fracture, and two cases of malunion. Sanders's score was applied to analyze the functional outcome among the cases. 63% of patients had excellent performance, 20% had good results, 13% had fair results and one patient performed poorly. Conclusion: MIPO is a good technique to stabilize the proximal tibia condyle fractures especially when used with meticulous intraoperative handling of soft tissues.
Keywords: MIPO, Proximal tibial condyle fractures, Invasive plate osteosynthesis
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Postgraduate Student, Department of Orthopaedics, C.U Shah Medical College and Hospital, Surendranagar, Gujarat, India. Email: |
Vora J, Shah J, Vala G. Functional outcome of minimally invasive plate osteosynthesis (MIPO) in proximal tibial fractures. Surgical Review Int J Surg Trauma Orthoped. 2020;6(2):110-120. Available From https://surgical.medresearch.in/index.php/ijoso/article/view/158 |


 ©
©