A Retrospective Analysis of Plate Fixation of Humerus Fracture
Kumar Kirar S.1, Upadhyay S.2*, Singh S.3, Varshney A.4
DOI: https://doi.org/10.17511/ijoso.2021.i02.06
1 Sunil Kumar Kirar, Senior Resident, Department of Orthopaedics, ABV Government Medical College, Vidisha, Madhya Pradesh, India.
2* Sanjay Upadhyay, Assistant Professor, Department of Orthopaedics, ABV Government Medical College, Vidisha, Madhya Pradesh, India.
3 Sanat Singh, Associate Professor, Department of Orthopaedics, ABV Government Medical College, Vidisha, Madhya Pradesh, India.
4 Atul Varshney, Professor & HOD, Department of Orthopaedics, ABV Government Medical College, Vidisha, Madhya Pradesh, India.
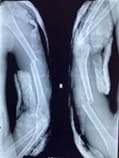
Introduction: Humeral shaft fractures represent 1–3% of all the fractures coming in our OPD. These fractures are mostly treated conservatively. Both the plate fixation and nailing techniques are being used but plate fixation has the advantage of lesser rates of malunion and non-union. Our study aimed to evaluate the results of plate fixation in our hospital that employs plate fixation as the golden standard. Materials and Methods: This was a retrospective cohort study of all patients treated for a humeral shaft fracture in our hospital (District Hospital Vidisha associated with ABV Medical College, Vidisha between July 2018 and June 2020 with a mean follow-up of 6 months. Results: Plate fixation was performed in 40 patients with a humeral shaft fracture. The mean age was 50 (SD 20) years with 60 % (n = 24) being male. There were 55 % (n = 22) fractures in the right and 45 % (n =18) fractures in the left. None of the patients develops superficial surgical site infection. Complications like Radial Nerve palsy, Deep surgical site infections and Non-union occurred in 2.5 % (n = 1), 2.5 % (n = 1) and 5 % (n = 2) of patients, respectively. The median duration of radiological fracture healing was 18 (range 10–42) weeks. Conclusion: Plate fixation for humeral shaft fractures has low risks of complications. The complications can be further minimized with greater surgical expertise.
Keywords: Plate fixation, Humerus shaft fracture, Complication
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Orthopaedics, ABV Government Medical College, Vidisha, Madhya Pradesh, India. Email: |
Kirar SK, Upadhyay S, Singh S, Varshney A, A Retrospective Analysis of Plate Fixation of Humerus Fracture. Surgical Rev Int J Surg Trauma Orthoped. 2021;7(2):28-35. Available From https://surgical.medresearch.in/index.php/ijoso/article/view/229 |


 ©
©