A rare case of osseous metaplasia in anaplastic thyroid cancer
N Wagh A.1, Samprathi D.2*, R Bhagvat S.3, Tandur A.4, N Dhimole N.5
DOI: https://doi.org/10.17511/ijoso.2021.i02.04
1 Amol N Wagh, Associate Professor, Department of General Surgery, Grant Government Medical College and JJ Group of Hospitals, Mumbai, Maharashtra, India.
2* Samprathi D, Resident, Department of General Surgery, Grant Government Medical College and JJ Group of Hospitals, Mumbai, Maharashtra, India.
3 Shirish R Bhagvat, Professor, Department of General Surgery, Grant Government Medical College and JJ Group of Hospitals, Mumbai, Maharashtra, India.
4 Amarjeet Tandur, Assistant Professor, Department of General Surgery, Grant Government Medical College and JJ Group of Hospitals, Mumbai, Maharashtra, India.
5 Nikhil N Dhimole, Resident, Department of General Surgery, Grant Government Medical College and JJ Group of Hospitals, Mumbai, Maharashtra, India.
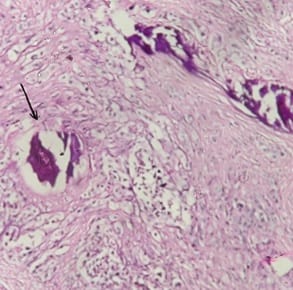
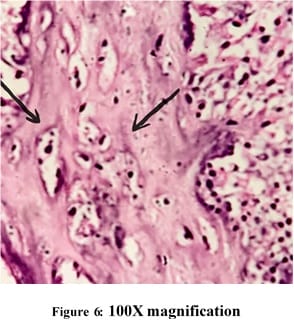
Anaplastic thyroid cancer is the most advanced and aggressive thyroid cancer. It is very rare and is found in less than 2% of patients with thyroid cancer. It most commonly occurs in people over the age of 60 years. It is usually diagnosed at later stages when the disease has already spread to surrounding structures or has grown large enough to compress the trachea or esophagus causing pressure symptoms. The patient here, a 75-year-old female, presented with a large swelling in the front of the neck in euthyroid status which was diagnosed as anaplastic thyroid cancer and was managed surgically and the surgical specimen was sent for histopathological examination. The presence of osseous metaplasia with mature bone formation in anaplastic thyroid carcinoma is a rare entity and has been discussed in this case report.
Keywords: Anaplastic, Thyroid, Neoplasm, Osseous, Metaplasia
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Resident, Department of General Surgery, Grant Government Medical College and JJ Group of Hospitals, Mumbai, Maharashtra, India. Email: |
Wagh AN, Samprathi D, Bhagvat SR, Tandur A, Dhimole NN. A rare case of osseous metaplasia in anaplastic thyroid cancer. Surgical Rev Int J Surg Trauma Orthoped. 2021;7(2):17-21. Available From https://surgical.medresearch.in/index.php/ijoso/article/view/222 |


 ©
©