Laparoscopic management of rare “ H type” duplication of gall bladder
Mishra A.1, Masud Ansari M.2, Misra S.3*
DOI: https://doi.org/10.17511/ijoso.2020.i06.03
1 Anurag Mishra, Senior Resident, Department of General Surgery, Dr. Ram Manohar Lohia Hospital, New Delhi, India.
2 Md Abu Masud Ansari, Associate Professor, Department of General Surgery, Dr. Ram Manohar Lohia Hospital, New Delhi, India.
3* Shivanshu Misra, Consultant Gastro, Laparoscopic Surgeon, Shivani hospital and IVF, Kanpur, Uttar Pradesh, India.
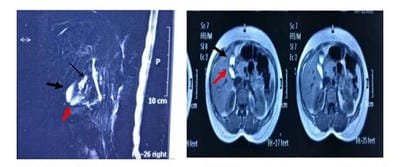
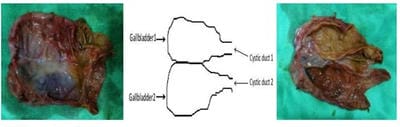
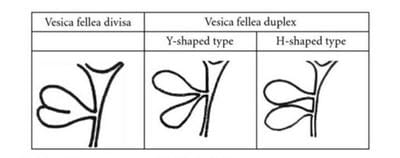
A duplicated gallbladder is a rare congenital anomaly with an incidence of 1:4000 live births. They can remain asymptomatic and identified incidentally or present as acute cholecystitis, empyema, torsion, cholecystoenteric fistula, Gall bladder lump, or carcinoma. Here the current case is about discussing a case of a 25-year-old female who presented with symptomatic gallstone disease with a duplicated gallbladder having multiple stones in both the gallbladders. MRCP performed preoperatively revealed Y type duplication (double Gall bladder with common cystic duct). Laparoscopic cholecystectomy was performed and it finally revealed H type duplication (double Gall bladder with separate cystic ducts for each Gall Bladder).
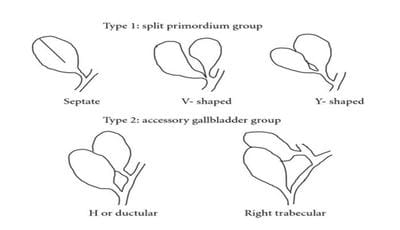
Keywords: Duplicated Gall Bladder, H type gall bladder, Boyden’s classification, Harlaftis classification
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Consultant Gastro, Laparoscopic Surgeon, Shivani hospital and IVF, Kanpur, Uttar Pradesh, India. Email: |
Mishra A, Ansari AM, Misra S. Laparoscopic management of rare “ H type” duplication of gall bladder. Surgical Rev Int J Surg Trauma Orthoped. 2020;6(6):353-356. Available From https://surgical.medresearch.in/index.php/ijoso/article/view/213 |


 ©
©