Importance of critical point of Sudeck in colorectal surgery: an anatomical study in cadaver
Jain P.1, Sharma D.2, Somashekar U.3, Kumar A.4*
DOI: https://doi.org/10.17511/ijoso.2020.i04.03
1 Pramesh Jain, Consultant, Cardio-thoracic and Vascular Surgery, Jabalpur, Madhya Pradesh, India.
2 Dhananjaya Sharma, Professor and Head, Department of Surgery, NSCB Medical College, Jabalpur, Madhya Pradesh, India.
3 Uday Somashekar, Associate Professor, Department of Surgery, NSCB Medical College, Jabalpur, Madhya Pradesh, India.
4* Atul Kumar, Assistant Professor, Department of Surgery, Government Medical College, Ratlam, Madhya Pradesh, India.
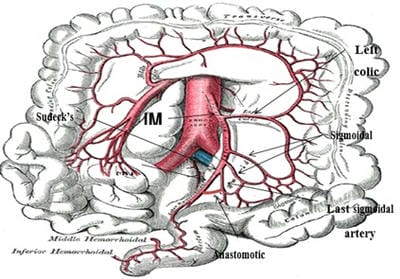
Background: To determine the incidence of the presence of a macroscopic anastomosis between the superior rectal artery and the last sigmoidal branch in a cadaveric population by means of macroscopic dissection. Also to measure the length of the inferior mesenteric artery from its origin from the abdominal aorta to Sudeck’s point and to determine the diameter of the anastomotic artery, if present. Material and Methods: Cadavers were dissected with midline vertical abdominal incision. After identifying the inferior mesenteric artery, it was ligated and divided from its origin as near as possible from the aorta. Results: Macroscopically looking for anastomosis between the superior rectal artery and the last sigmoid artery and measured its diameter. Among 40 cadavers, 34 were males and 6 were females. A macroscopic anastomosis between the superior rectal artery and the last sigmoid artery could be identified in 32 (80.0%) and was absent in 8 (20.0%). The mean length was 43.6 (±.46) mm from the origin of the inferior mesenteric artery to Sudeck’s point. The mean diameter of this anastomotic vessel was 1.9 (±0.65) mm. Conclusion: Sudeck’s point may be considered important during surgery because of the uncertainty of the presence of a macroscopic anastomosis between the superior rectal artery and the last sigmoidal artery (absent in 20.0%) and small diameter of the anastomotic vessel which fulfill the need of the caudal stump.
Keywords: Sudeck’s point, Macroscopic anastomosis, Superior rectal artery
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Surgery, Government Medical College, Ratlam, Madhya Pradesh, India. Email: |
Jain P, Sharma D, Somashekar U, Kumar A. Importance of critical point of Sudeck in colorectal surgery: an anatomical study in cadaver. Trauma and Orthopedics. 2020;6(4):237-243. Available From https://surgical.medresearch.in/index.php/ijoso/article/view/193 |


 ©
©