Gallbladder retrieval through an epigastric and umbilical port in laparoscopic cholecystectomy- a comparative study
Sainia T.1, Kumar Golandaj V.2*, Kumar Malviya V.3
DOI: https://doi.org/10.17511/ijoso.2020.i03.02
1 Tarun Sainia, Associate Professor, Department of General Surgery, L.N. Medical College and J.K. Hospital, Bhopal, Madhya Pradesh, India.
2* Vinay Kumar Golandaj, Resident, Department of General Surgery, L.N. Medical College and J.K. Hospital, Bhopal, Madhya Pradesh, India.
3 Vikas Kumar Malviya, Associate Professor, Department of General Surgery, L.N. Medical College and J.K. Hospital, Bhopal, Madhya Pradesh, India.
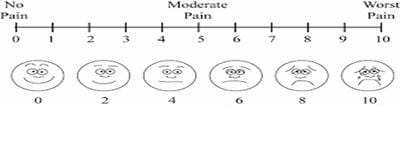
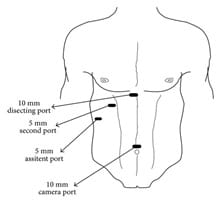
Aim: This comparative prospective study was conducted at the L.N. Medical College and J.K. Hospital Bhopal Madhya Pradesh for a period of one year from Jan 2019 to Dec 2019. Material and Methods: The study included 100 patients who underwent planned four-port laparoscopic cholecystectomy for symptomatic, asymptomatic cholelithiasis, and benign gall bladder diseases. These patients were randomly divided into two groups. The first 50 patients in whom GB was retrieved from Epigastric port were assigned in Group A and the other 50 patients where GB was retrieved from Umbilical port were assigned in Group B. The fascial defect of a 10 mm port was closed by vicryl "2.0" with a port closure needle, while three 5 mm ports closed by applying sterile small dressing. Both groups use a surgical glove endobag for gall bladder retrieval. Results: The results of both these techniques were collected and analyzed. The mean age of patients was 43.8 years in group A and 43.6 in group B. The male to female ratio was near 1:2. in both groups. Group A VAS score is 4.2 and while in group B 3.1.Conclusion: Post-operative port site infection in group A was 2% while in group B is 4%, post-operative port site scar was cosmetically better and satisfactory in umbilical port than epigastric port.
Keywords: Gallbladder, Laparoscopic cholecystectomy, Port site infection, Visual analog score
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Resident, Department of General Surgery, L.N. Medical College and J.K. Hospital, Bhopal, Madhya Pradesh, India. Email: |
Sainia T, Golandaj VK, Malviya VK. Gallbladder retrieval through an epigastric and umbilical port in laparoscopic cholecystectomy- a comparative study. Surgical Review Int J Surg Trauma Orthoped. 2020;6(3):147-153. Available From https://surgical.medresearch.in/index.php/ijoso/article/view/177 |


 ©
©