Evaluation of factors determining the functional outcome of DHS in trochanteric fractures
Deshpande S.1, R Agrawal S.2*
DOI: https://doi.org/10.17511/ijoso.2020.i02.03
1 Santosh Deshpande, Assistant Professor, Department of Orthopaedics, Ashwini Rural Medical College, Hospital and Research Centre, Kumbhari, Maharashtra, India.
2* Saurabh R Agrawal, Consultant, Agrawal Nursing Home, Solapur, Maharashtra, India.
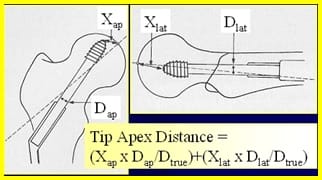
Background: In spite of improvement and modification for intertrochanteric fracture in the conservative line of treatment the ideal anatomical and functional result could not be achieved.Until now mentioned factors posteromedial support communition has been considered to bea major prognostic factor in the determination of the functional outcome. Current literature almost neglects other important potential prognostic factor i.e. lateral trochanteric wall fracture.The current study has aimed at studying Assessment of functional outcomes of Dynamic Hip screw fixation in intertrochanteric fracture Evans 3 and 4 types. Method: 126 cases were registered in the study out of which 64 cases of Trochanteric fractures which were admitted in the Orthopaedic wards and treated by internal fixation using standard Dynamic Hip Screw (DHS) were included in the study. Preoperative assessment of fracture geometry was done using Evan’s classification. Result: Age of patients ranged from 22 years to 88 years, with the average being 55 yrs. the anatomical reduction was achieved in 82.5% of group A with intact lateral trochanteric wall whereas it was achieved in only 33% of the other group. Average impaction in group A was found to be 5.5mm and average impaction in group B was 14mm. 85% of group A had functional outcome excellent to good whereas in 66% of group B it was fair to poor. Conclusion: Intact lateral trochanteric wall helps in achieving anatomical reduction, imparts inherent stability and prevents excessive collapse, limb shortening and sliding of the screw. Thus it helps in achieving good functional outcome making lateral trochanteric wall fracture good predictor of functional outcome.
Keywords: Trochanteric fracture, Dynamic Hip Screw (DHS), Evan’s classification, Functional outcome
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Consultant, Agrawal Nursing Home, Solapur, Maharashtra, India. Email: |
Deshpande S, Agrawal SR. Evaluation of factors determining the functional outcome of DHS in trochanteric fractures. Surgical Review Int J Surg Trauma Orthoped. 2020;6(2):79-86. Available From https://surgical.medresearch.in/index.php/ijoso/article/view/167 |


 ©
©