Bipolar hemiarthroplasty versus total hip replacement in displaced femoral neck fracture in elderly
Choudhary MB.1, Ram GG.2*
DOI: https://doi.org/10.17511/ijoso.2020.i02.07
1 Mohan B Choudhary, Associate Professor, Department of Orthopaedics, Sri Ramachandra Medical College, Chennai, Tamil Nadu, India.
2* Ganesan G Ram, Associate Professor, Department of Orthopaedics, Velammal Medical College, Madurai, Tamil Nadu, India.
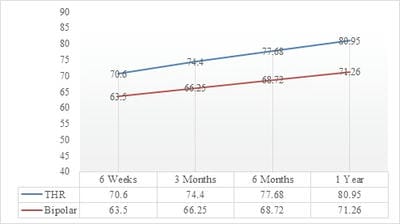
Introduction: Fractures of the neck of the femur are commonly seen in the geriatric population resulting in significant morbidity and mortality. Primary arthroplasty helps in rapid mobilization while decreasing the chances of implant failure and complications such as deep vein thrombosis, pulmonary complications, infection, and bedsores. The purpose of this can be fulfilled either by Bipolar Hemiarthroplasty as well as by Total Hip arthroplasty. The aim of this study is to determine whether total hip replacement is clinically and functionally better than bipolar hemiarthroplasty in the neck of femur fracture in older patients. Method: It is a prospective study done at Sri Ramachandra Medical College, Chennai, and Velammal Medical College, Madurai on 70 patients diagnosed with the unstable neck of femur fractures who were treated with bipolar hemiarthroplasty and total hip replacement from April 2018 to September 2019. The inclusion criteria were age more than 60 years and Unstable neck of femur fractures as per the Garden classification. The exclusion criteria were pathological fractures, associated fracture of lower limbs, and non-ambulatory patients prior to the injury. A functional assessment was carried out using the Harris Hip Score. Results: In the group that underwent a total hip replacement, the mean Harris Hip Score was 70.6, 74.4, 77.68 and 80.95 at the follow-up visits at week 6, 3 months, 6 months and 1 year respectively. In the group that underwent bipolar hemiarthroplasty, the mean Harris Hip Scores were 63.50, 66.25, 68.72, and 71.26 at the follow-up visits at week 6, 3 months, 6 months and 1 year respectively. Conclusion: Total hip arthroplasty is recommended over hemiarthroplasty for the displaced neck of femur fractures in elderly patients owing to the higher Harris Hip Scores and lower re-operation rates.
Keywords: Neck of the femur, Bipolar Hemiarthroplasty, Harris Hip score, Osteoporosis, Total Hip replacement
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Associate Professor, Department of Orthopaedics, Velammal Medical College, Madurai, Tamil Nadu, India. Email: |
Choudhary MB, Ram GG. Bipolar hemiarthroplasty versus total hip replacement in displaced femoral neck fracture in elderly. Surgical Review Int J Surg Trauma Orthoped. 2020;6(2):105-109. Available From https://surgical.medresearch.in/index.php/ijoso/article/view/166 |


 ©
©