A rare complication of ERCP: colocutaneous fistula
Mishra N.1, Goyal S.2*
DOI: https://doi.org/10.17511/ijoso.2020.i02.11
1 Navneet Mishra, Associate Professor, Department of General Surgery, L.N. Medical College and J.K. Hospital, Bhopal, Madhya Pradesh, India.
2* Sakshi Goyal, PG Resident, Department of General Surgery, L.N. Medical College and J.K. Hospital, Bhopal, Madhya Pradesh, India.
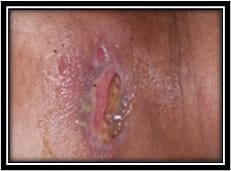
Endoscopic Retrograde Cholangiopancreatography (ERCP) is the most widely used diagnostic and therapeutic modality for hepatobiliary and pancreatic diseasesbut is not free from complications. Though rare, the common complications are migration of biliary stent, perforation, pancreatitis, hemorrhage, cholangitis, intra-abdominal sepsis, obstruction, etc. Here, we report a rare complication of ERCP presented as colocutaneous fistula. Colocutaneous fistulas are abnormal communications between the colon and the abdominal skin. They can occur spontaneously in patients with inflammatory bowel disease (most common) as well as after an injury or a surgical procedure. About one-third of fistulas close spontaneously with medical treatment and surgery being reserved for failures after optimal medical treatment. This case of colocutaneous fistula following ERCP presented to us was successfully treated as a single staged procedure without any complication. To the best of our knowledge, this is the first case reported of colocutaneous fistula following ERCP.
Keywords: ERCP, Colocutaneousfistula, Single staged procedure
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , PG Resident, Department of General Surgery, L.N. Medical College and J.K. Hospital, Bhopal, Madhya Pradesh, India. Email: |
Mishra N, Goyal S. A rare complication of ERCP: colocutaneous fistula. Surgical Review Int J Surg Trauma Orthoped. 2020;6(2):134-138. Available From https://surgical.medresearch.in/index.php/ijoso/article/view/154 |


 ©
©